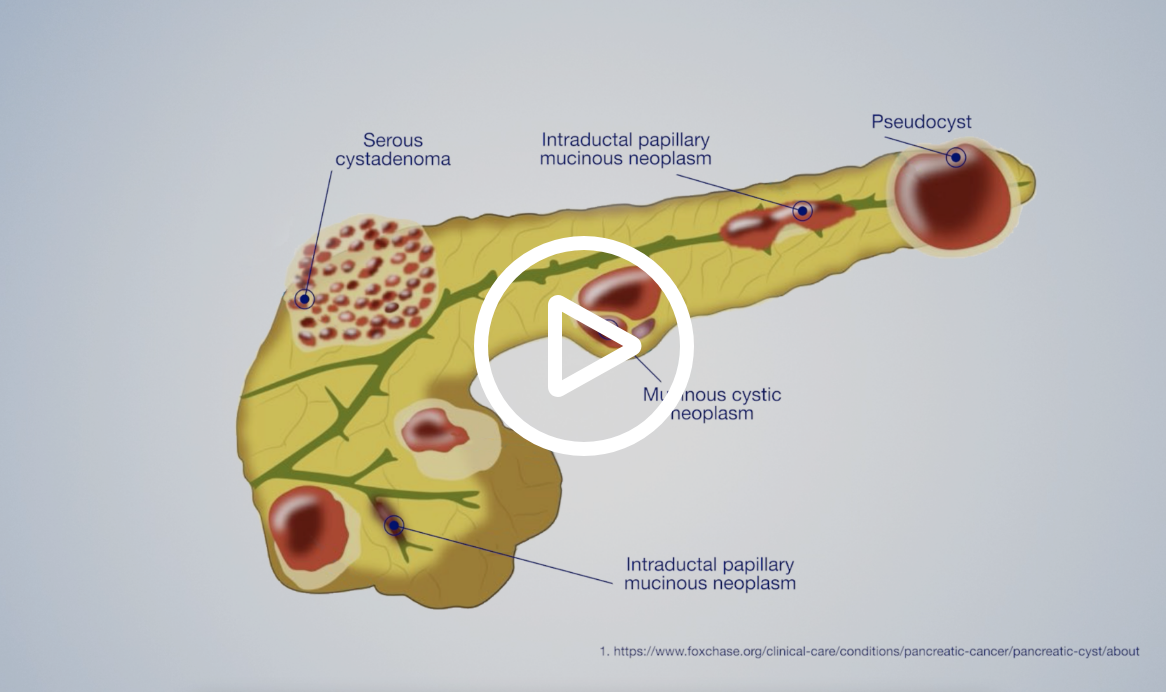
Pancreatic cancer occurs when cells go through changes that cause them to behave differently than normal cells. These abnormal cells then grow and divide at a rapid rate, and may form a mass or tumor.
Pancreatic tumors can fall into one of three categories: benign, precancerous or malignant.
Benign Tumors
Benign tumors are noncancerous and do not spread. However, benign tumors can become malignant over time. Common tumor types include serous cystic neoplasms, and pseudocysts or inflammatory masses from pancreatitis, which is inflammation of the pancreas.
Precancerous Tumors
Precancerous tumors are not cancerous yet, but if left untreated, may become cancerous. Common tumor types include intraductal papillary mucinous neoplasms (IPMN) and mucinous cystic neoplasms.
Malignant Tumors
A malignant tumor is cancerous. Malignant tumor cells can grow quickly and spread throughout the body. When the malignant cells spread, this is called metastasis.
Types of Pancreatic Cancer
For more information on types of pancreatic cancer, speak with your physician.
Exocrine Tumors
The majority of pancreatic tumors are exocrine tumors. The most common type of exocrine tumor is pancreatic adenocarcinoma or pancreatic ductal adenocarcinoma, accounting for approximately 90% of pancreatic cancer cases. There are other, rare types of exocrine tumors; some include acinar cell carcinoma, mucinous cystic neoplasms, and squamous cell carcinoma.
Neuroendocrine Tumors
Pancreatic neuroendocrine tumors (pNET) account for approximately 7% of pancreatic cancer cases. These tumors begin in the hormone-producing (islet) cells. pNETs can be functional or nonfunctional. Functional tumors over-produce hormones, while nonfunctional tumors do not produce hormones. Most pNETs are nonfunctional. Insulinoma, gastrinoma, glucagonoma and nonfunctional islet cell tumors are types of pancreatic neuroendocrine tumors.
Pancreatic Cancer Risk Factors
![]()
Pancreatitis
Pancreatitis is inflammation of the pancreas and can be chronic or acute. Acute pancreatitis usually occurs suddenly and resolves within a few days. Chronic pancreatitis is inflammation that does not improve but gets worse over time. This leads to permanent damage of the pancreas and increases the risk of developing pancreatic cancer. Those with hereditary pancreatitis have an even higher risk of developing pancreatic cancer.7
Family History
Approximately 5-10% of pancreatic cancer cases are linked to family history or an inherited gene mutation.3 People with two or more first-degree relatives (parent, sibling, child) with pancreatic cancer or a first-degree relative who developed pancreatic cancer before the age of 50, have an increased risk of developing pancreatic cancer themselves.3 Inherited genetic mutations, such as LKB1/STK11 (Peutz-Jeghers syndrome), CDKN2A (FAMMM), BRCA2, BRCA1, PALB2, ATM, MLH1, MSH2, or MSH6, can also increase the risk of developing pancreatic cancer.1 According to the National Comprehensive Cancer Network Guidelines for Pancreatic Cancer, germline testing is recommended for anyone with confirmed pancreatic cancer.14
Diabetes
Diabetes is a risk factor and can also be a complication of pancreatic cancer.4 Pancreatic cancer is more likely to occur in people who have long-standing (over 5 years) diabetes. Early onset diabetes in people 50 years or older, could be an early sign of pancreatic cancer.4
Obesity
Obesity is defined as a body mass index (BMI) of 30 and above.6 Studies have shown a link between obesity and pancreatic cancer, and an increased risk of developing the disease.6 In addition, those who are obese in early adulthood have an even greater risk of pancreatic cancer and a lower overall survival rate.6
Smoking
Tobacco smoking is considered an important risk factor of pancreatic cancer.2 People who smoke cigarettes are more likely to develop pancreatic cancer than people who have never smoked.2 The risk decreases with smoking cessation, but former smokers are still more likely to develop pancreatic cancer than those who have never smoked.2
Alcohol
There is research that suggests heavy alcohol consumption may increase the risk of pancreatic cancer. Heavy drinkers are more likely to develop pancreatic cancer than those who never drink.2 Heavy drinking is defined as consuming more than 3 alcoholic beverages per day.2
Age
The chance of developing pancreatic cancer increases with age. Most people diagnosed with pancreatic cancer are between the ages of 60 and 80 years old.7
To better understand your risk, please consult your physician to determine whether a referral to a specialist or genetic counselor is appropriate.Get Screened |
Pancreatic Cancer Symptoms
Unfortunately, pancreatic cancer symptoms are vague and usually do not appear until the disease is more advanced. It is known to be a silent disease. Symptoms can include the following:
Diagnosing Pancreatic Cancer
If you have symptoms, your physician will review your medical history, perform a physical, and order tests. The imaging tests below are the most common to evaluate the pancreas. If the imaging test results suggest an abnormality in your pancreas, your physician will likely order further tests that commonly include obtaining a tissue sample by biopsy.

Endoscopic Ultrasound
Endoscopic Ultrasound or EUS is a procedure that uses an endoscope, with an ultrasound transducer at the tip, that allows the physician to see beyond the digestive tract to visualize all five wall layers as well as surrounding tissue and organs. The physician can assess tumors and determine if cancer has spread. They are also able to obtain a tissue biopsy during the procedure.

Magnetic Resonance Imaging
Magnetic Resonance Imaging (MRI) uses radio waves and magnets to take cross-sectional images of organs and structures inside the body. An MRI can show if there is a tumor and its location.

Positron Emission Tomography
A positron emission tomography (PET) scan uses radiation to view cellular activity within the body. A radiotracer is injected into the body and images of the radioactivity are collected. The radioactive substance is drawn to cancer tumors, which typically appear brighter on the images. While a PET scan is less likely to be used to diagnose cancer, it can be used to determine where the primary cancer is located, and if cancer has spread. It can also be used to see if chemotherapy is working.

Computed Tomography
A Computed Tomography (CT) or Computed Axial Tomography (CAT) scan takes cross-sectional X-rays (slices) of the body and compiles the data to produce a detailed image. A CT scan can show if a tumor is present and where it is located.
| Imaging Test | Pros | Cons |
|---|---|---|
| EUS (Endoscopic Ultrasound) |
|
|
| CT (Computed Tomography) Scan |
|
|
| MRI (Magnetic Resonance Imaging) |
|
|
| PET (Positron Emission Tomography) |
|
|
EUS (Endoscopic Ultrasound)
Pros:
- Close proximity to the pancreas, enabling the physician to visualize pancreatic tumors and determine size and location
- Higher image resolution and detection rates of small lesions when compared to CT and MRI.8,9
- Able to obtain a tissue biopsy during the exam, allowing for accurate staging of pancreatic cancer
- If pancreatic cancer, able to provide accurate staging
- Can visualize other organs to check if the cancer has spread
- No radiation
Cons:
- Sedation required
- Potential complications (very rare): bleeding, perforation, infection, pancreatitis
CT (Computed Tomography) Scan
Pros:
- Images the pancreas well
- Can determine tumor size and location
- Can detect an abnormal area of the pancreas
- Helps determine if disease has spread
- Relatively quick
Cons:
- Can miss small lesions
- Radiation
- Difficult biopsy access
- Requires breath holding
- Artifacts from metal
- Contrast, if needed, cannot be used for all patients due to allergies and chronic kidney issues
MRI (Magnetic Resonance Imaging)
Pros:
- High quality images of pancreas and biliary system
- No radiation
Cons:
- May trigger claustrophobia
- Magnetic field, which may prevent patients with metal hardware from having an exam
- Must remain still
MRI (Magnetic Resonance Imaging)
Pros:
- Helps determine if disease has spread
- Can also be used to see if chemotherapy is working
- When combined with CT, it provides a good picture of the patient’s condition
Cons:
- Radiation
- Injected radiotracer may not be suitable for all patients (pregnant, breastfeeding, allergies)
- Radioactivity post scan can pose a small risk to others
- Cannot detect exact location of cancer
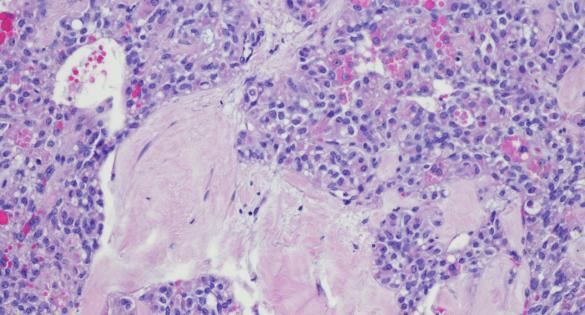
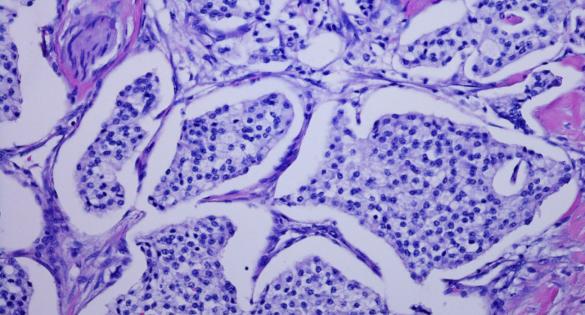
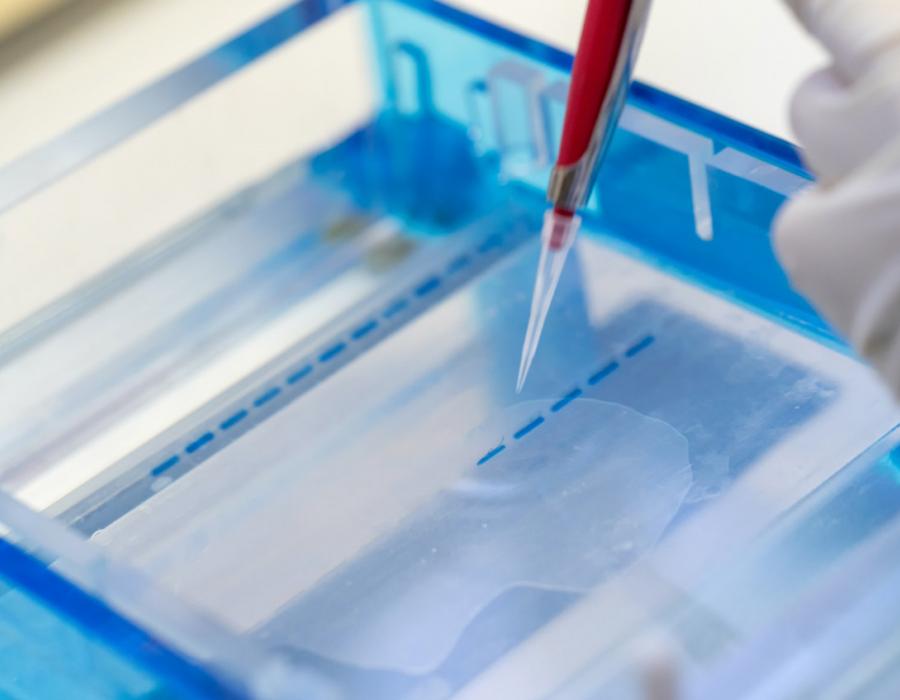
Biopsy
To confirm if a tumor is cancerous and determine the best treatment option, your physician will need a tissue sample or biopsy. These tissue samples are then examined under a microscope. For pancreatic cancer, this biopsy is usually performed during an endoscopic ultrasound (EUS) procedure.
EUS-guided fine-needle biopsy (FNB) is performed in many large medical centers as part of routine gastrointestinal cancer staging. The EUS image helps the physician see where to place the biopsy needle to remove tissue from the region of interest.
EUS-FNB aids in the diagnosis and staging of malignant diseases (tumors and metastasis) or provides further assessment of benign diseases through tissue acquisition. EUS-FNB can provide detailed molecular information to your physician that can potentially help shape treatment options.
Molecular Profiling
Molecular profiling is when a tissue sample is examined to identify unique characteristics of a tumor, such as genetic mutations and biomarkers.
A group of people can all be diagnosed with pancreatic cancer, but their cancer cells may have different genetic make-up. Understanding the genetic characteristics associated with the cancer calls, may help determine a treatment plan that works best.
Pancreatic Cancer Staging
Physicians consider the following information to determine cancer stage and if it can be surgically removed or not. This information helps determine prognosis and the treatment plan.
What is the size of the tumor and has it grown outside of the pancreas?
Has it spread to nearby lymph nodes and how many?
Has it spread to nearby blood vessels?
Has it spread to other organs or distant lymph nodes?
Stage I
The tumor is contained within the pancreas and has not spread to other lymph nodes, organs or blood vessels. Stage I can be further characterized into Stage IA and Stage IB. Stage IA is when tumors are 2cm or less in size, and stage IB is when tumors are between 2-4cm in size. Stage I tumors are usually resectable, meaning they can be surgically removed.
Stage II
The tumor has spread outside the pancreas, to nearby blood vessels and/or lymph nodes (no more than 3). Again, there are two sub-stages within Stage II; Stage IIA and Stage IIB. In Stage IIA, the tumor is larger than 4cm but has NOT spread to nearby lymph nodes. In Stage IIB, the tumor HAS spread to nearby lymph nodes. Stage II tumors can be resectable or borderline resectable. Borderline rectable tumors may not be able to be surgically removed as they may have just spread to nearby blood vessels.
Stage III
The tumor has either spread to 4 or more nearby lymph nodes or grown into a major blood vessel but has not spread to another part of the body. Stage III tumors are usually unresectable, meaning they cannot be removed by surgery.
Stage IV
The cancer has metastasized, or spread, to another part of the body, such as the liver, lungs, bones or abdominal wall. The tumor(s) may be any size and may or may not have spead to nearby lymph nodes. This stage is also called metastatic cancer and is unresectable.
Pancreatic Cancer Treatments
Chemotherapy
Chemotherapy is when a drug is administered to fight cancer cells. These anti-cancer drugs can be given through an IV or by mouth and travel through the bloodstream throughout the body. Chemotherapy can be used in combination with other treatment options.
Radiation Therapy
Radiation therapy is when high-energy waves are focused on the affected area to damage cancer cells. Like chemotherapy, it can be used with other treatment options. It can help shrink the tumor, damage any remaining cancer cells after surgery or relieve pain caused by the tumor.
Surgical Resection
Surgical resection is when the tumor is removed from the body. Typically this is only performed if the entire tumor can be removed. The procedure and recovery are long and complex, but it is often the best option for a chance to cure pancreatic cancer.

Learn more about Olympus’ EUS, ERCP, and Surgical products that aid in the diagnosis and treatment of pancreatic cancer.
1. Management of patients with increased risk for familial pancreatic cancer: updated recommendations from the International Cancer of the Pancreas Screening (CAPS) Consortium: Goggins M, et al. Gut 2020;69:7–17. doi:10.1136/gutjnl-2019-319352
2. TOBACCO AND ALCOHOL AS RISK FACTORS FOR PANCREATIC CANCER: Best Pract Res Clin Gastroenterol. Author manuscript; available in PMC 2018 October 01.
3. Epidemiology of pancreatic adenocarcinoma: Chin Clin Oncol 2017;6(3):24
4. Risk factor, early diagnosis and overall survival on outcome of association between pancreatic cancer and diabetes mellitus: Changes and advances, a review: International Journal of Surgery 52 (2018) 342–346
5. Pancreatic Cancer Genetics: http://www.ijbs.com
6. Obesity and Pancreatic Cancer: Overview of Epidemiology and Potential Prevention by Weight Loss: Pancreas. Author manuscript; available in PMC 2019 February 01.
7. Epidemiology of pancreatic cancer: www.wjgnet.com, November 28, 2016, Volume 22, Issue 44
8. Palazzo L, Roseau G, Gayet B, et al. Endoscopic ultrasonography in the diagnosis and staging of pancreatic adenocarcinoma. Results of a prospective study with comparison to ultrasonography and CT scan. Endoscopy 1993;25:143-50
9. Fusaroli P, Kypraios D, Caletti G, et al. Pancreatico-biliary endoscopic ultrasound: a systematic review of the levels of evidence, performance and outcomes. World J Gastroenterol 2012;18:4243-56
10. American Cancer Society
11. Pancreatic Cancer Action Network
12. American Society for Gastrointestinal Endoscopy
13. National Cancer Institute
14. National Comprehensive Cancer Network