Endoscopic ultrasound or EUS combines ultrasound technology with endoscopy to take ultrasound images from within the body.
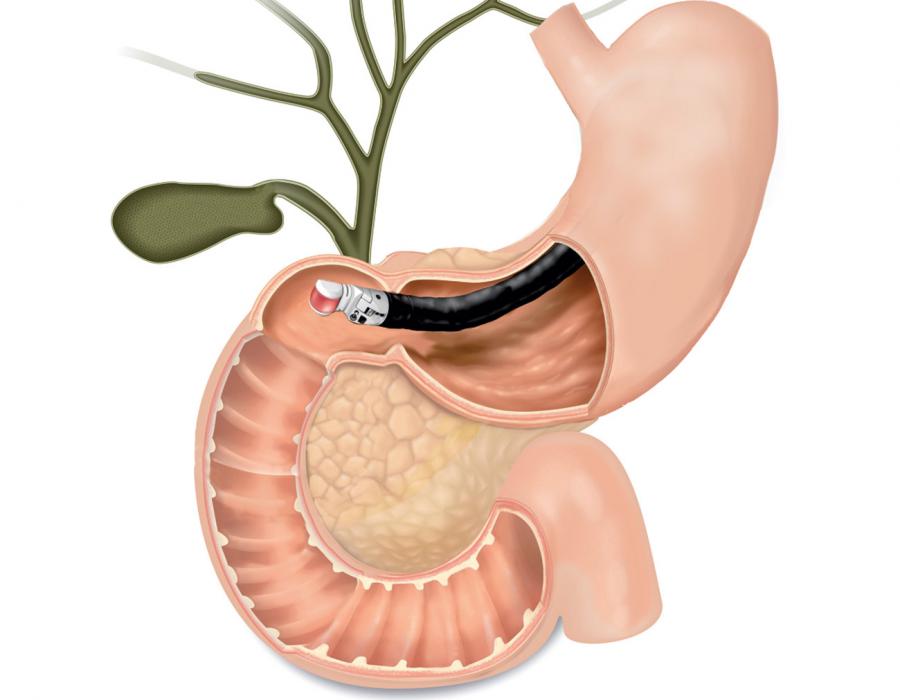
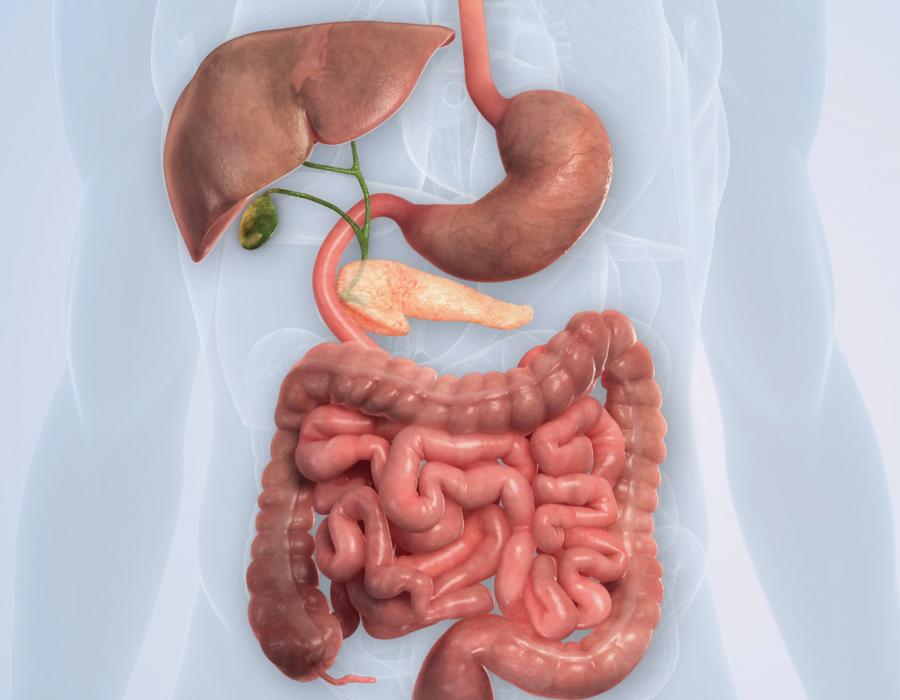
A scope or thin tube, with a camera and ultrasound probe at the end, is inserted into the mouth and down the esophagus to the stomach and intestine, allowing a physician to view beyond the digestive tract wall. The physician can then visualize the tissues and organs that surround the tract, which includes the pancreas.
Close proximity to the pancreas
During an endoscopic ultrasound (EUS) procedure, the physician is able to place the scope very close to the pancreas. This allows the physician to see tumors within the pancreas and determine their size and location. It is difficult to access and visualize the pancreas from the outside of the body using conventional ultrasound since the pancreas sits behind the stomach.

High resolution images
Endoscopic ultrasound (EUS) allows the physician to see small lesions, which can be less than 3cm in size due to the high image resolution and close proximity to the pancreas. EUS can also detect smaller lesions more often, when compared to MRI and CT.8,9
Able to obtain a tissue biopsy
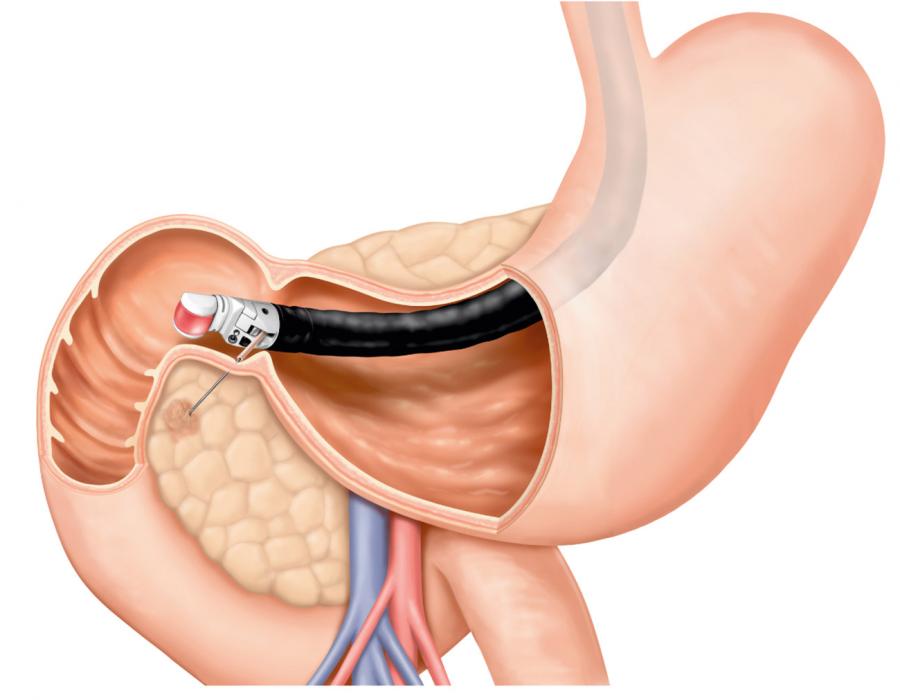
Obtaining a tissue sample with a biopsy needle allows the physician to diagnose and stage the cancer. The biopsy occurs during the EUS procedure, while the patient is sedated. Using ultrasound guidance, the needle goes through the scope and into the tumor. The information from the tissue biopsy is important to determine the best treatment option.
Can visualize other organs to check if the cancer has spread
The EUS scope is inserted into the digestive tract to see tissues and organs beyond the tract wall. Some of the organs that can be visualized with EUS are the pancreas, liver, spleen, gallbladder and lymph nodes. Since all of these areas can be seen during an EUS procedure, the physician can do a full examination and determine if the cancer has spread beyond the pancreas.
No radiation
Unlike CT, ultrasound provides high resolution imaging of anatomy using sound waves, without the need for radiation.


What Can I Expect from
My EUS Procedure?
During an EUS procedure, the physician is able to place the scope very close to the pancreas. Anatomically, the pancreas is situated just behind your stomach and right in front of your spine. Therefore, an endoscope placed in your stomach and in the first part of your small intestine allows for easy visualization of your entire pancreas with an ultrasound probe located at the tip of the endoscope. Because the ultrasound probe is so close to the pancreas, the physician is able to see tumors within the pancreas and determine their size and location.
He or she can determine whether the tumor has grown beyond the pancreas and if it has touched other vital structures that may influence treatment. It is also possible to detect lymph nodes that may be enlarged due to tumor spread. Access to and visualization of the pancreas from the outside of the body is difficult using conventional ultrasound since the pancreas sits behind the stomach. Interfering gas in the stomach can prevent clear visualization of the pancreas, and the increased distance of the pancreas from the ultrasound probe makes a needle biopsy more challenging.

Your physician likely ordered an EUS exam based on, one or a combination of, the following: symptoms, blood test results and/or results of other procedures, such as a CT scan or MRI. If a tumor is suspected to be present in the pancreas, the physician will be able to visualize and evaluate it, as well as surrounding organs with EUS. For instance, a large portion of the liver can also be visualized to look for any concerning lesions. It is important to define not just the nature of a pancreatic mass, but also the extent of the tumor’s involvement with other structures.
Preparing for the day of the procedure
To make the procedure comfortable and safe for you, an EUS procedure is typically performed with some type of sedation or anesthesia. Commonly, an anesthesiologist (a physician who specializes in delivering anesthesia) will be present. It is important that your stomach be empty before the procedure to prevent any complications like vomiting due to the endoscope or the anesthesia. Food also interferes with ultrasound visualization. For these reasons, you will be asked to fast for at least eight hours prior to your procedure time (typically nothing to eat after midnight).
Most anesthetic medications used for this procedure are short-acting and will resolve within 2-4 hours after the procedure. This can leave you feeling some grogginess upon waking up. Therefore, most facilities require that you not operate a vehicle that day and should plan on having someone drive you home. If you do not have a ride home, your procedure will likely be rescheduled. In some cases, there are specially licensed drivers who can bring you home. Please check with your facility in advance.
The procedure time itself can vary between 20 minutes to an hour depending on whether a biopsy will be performed. In total, you can expect the time from when you arrive until the time you leave the facility, to be approximately three to four hours.
I have arrived for my procedure. What happens now?
Once you arrive, you will check in at the reception desk. They will go over your contact information and any last-minute insurance related information. You will then be taken into a pre-procedure area by a nurse or medical assistant. You will be asked to change into a hospital gown and then a nurse will review standard information in preparation of your procedure, including current medications and allergies, along with ensuring you have secured transportation home. They will also provide you with contact information in case you need to get in touch with the doctor after the procedure.
After this process is completed, the gastroenterologist performing your procedure will meet with you and make sure you are ready for the procedure. This includes addressing any questions you have about the procedure, and then going over the risks and benefits of proceeding with the procedure. You will then be asked to give your consent or permission to perform the procedure by signing an informed consent document. Again, all potential risks and/or complications will be discussed with you at that time. Complications from an EUS procedure are rare but may include bleeding from the biopsy site, infection, pancreatitis (inflammation of the pancreas) or perforation (tear in the lining of the GI tract that requires repair).
If your procedure will include the services of an anesthesiologist (in some cases, a nurse can provide adequate sedation under the supervision of the gastroenterologist doing the procedure), he or she will visit you to review the anesthesia plan and address any questions you may have. The type of sedation used at each facility may vary from “conscious sedation” (partially awake, but you will not feel pain or remember the procedure afterwards) to general anesthesia with intubation (rare for this procedure). Typically, MAC or Monitored Anesthesia Care is used. MAC is similar to, but in a deeper sleep than conscious sedation, you will not remember the procedure nor will you feel pain.
As noted above, the procedure typically ranges from 20 to 60 minutes. During the procedure, the doctor may find it necessary to perform a biopsy. He or she can visualize the area of interest and then obtain a tissue sample using a needle. The needles used for sampling are no larger than the needles commonly used for an IV. Under ultrasound guidance, the needle will be visualized passing through the stomach or small intestine wall and into the region of concern within your pancreas. This is typically referred to as fine-needle biopsy (FNB) or fine-needle aspiration (FNA). The sample is then tested in the lab for any abnormalities, such as cancer. These results are often not finalized by the end of the procedure, but in some cases, a preliminary result can be given. Your physician will update you on the status of this in the recovery area.
My procedure is over. Will I be in pain and how do I find out about my results?
After the procedure, you will be monitored in the recovery area for 30 to 60 minutes by a trained nurse. There is a possibility of feeling soreness in the throat due to the passage of the scope. If you experience this, it is often mild and rarely needs to be treated. Over-the-counter sore throat drops can help if desired, but often are not necessary. You will also likely feel tired. If a biopsy was performed, it may take up to two weeks for the lab to process the tissue sample. The physician will let you know when you might expect the results and if a preliminary result is available. The timeline varies among facilities, so asking your physician how long it will take at your specific facility is recommended.
Your physician will want to follow up with you to discuss results and if necessary, a treatment plan. This usually happens within a week or two of the procedure. Again, this varies among facilities, so confirming a follow up plan with your physician is recommended.